Addressing America’s Rural Mental Health Care Crisis
By Former U.S. Senator Heidi Heitkamp, One Country Project Founder and Chair
The U.S. is in the midst of an ongoing mental health crisis, with one in four adults impacted. Unfortunately, rural communities, in particular, often lack access to mental health care services and need congressional support to help close this gap. There isn’t a family in rural America – including my own – that isn’t touched by this crisis.
While in office, I introduced legislation to address the impacts of childhood trauma and improve mental health resources for rural veterans, but challenges remain. We need to continue shifting the mental health narrative to encourage rural communities to seek care and ensure adequate funding and resources are allocated to do so.
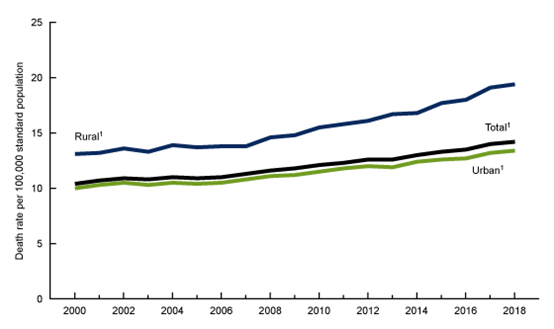
As I discussed on One Country Project’s podcast, “The Hot Dish,” this May, these issues are multifaceted and echo a much broader national crisis. For example, the ongoing opioid epidemic and limited broadband access to receive telehealth services have all contributed to the mental health crisis in rural areas. According to research from the Centers for Disease Control and Prevention (CDC), rural suicide rates have increased by nearly 50% over the past two decades compared to urban rates increasing by 34%, accelerating the disparity between the two. Lives are lost every day, offering a stark reminder that Washington must step up and support rural America.
The ongoing shortage of mental health professionals has only exacerbated this issue. It’s no secret we need to expand our mental health workforce, but it’s often overlooked that 61% of these shortages are in rural areas. When rural residents take the brave step of seeking help, they often find that they can’t get it. According to the North Dakota Pediatric Mental Health Access Program, 48 of our 53 counties don’t have enough mental health professionals to treat their needs, and in the five that do, waiting lists are several months long. Telehealth offers promising solutions here, but more must be done to expand access, such as ensuring sufficient broadband coverage and funding rural mental health programs and outreach initiatives. Additional flexibilities are needed to make sure people who need it most can access these services.
Even so, telehealth alone cannot solve this crisis. Programs that incentivize mental health professionals to practice in rural regions can help with staffing shortages. Studies have shown that completing their residency in a rural area makes professionals more likely to stay long-term and loan forgiveness programs such as the Substance Use Disorder Treatment Recovery (STAR) Loan could help minimize the workforce retention challenges in rural and underserved communities. But there’s still a systemic problem stemming from inadequate reimbursement for behavioral services. As hospitals and health systems in rural areas face continued financial pressures, recruiting and retaining those workers becomes difficult.
While we work to bolster the rural health care workforce, we must also ensure patients have access to effective treatments for the opioid crisis, as most are unaware that proper medical treatments exist. While steps have been taken to increase access to buprenorphine and other opioid use disorder treatments, more education is needed to reduce the stigma surrounding these vital treatments.
Perhaps nowhere else can the direct results of a broken mental health care system be better seen than in hospital emergency room departments across rural America. The chronic underfunding for behavioral health services has left individuals in serious mental health crises, their families and law enforcement officials with limited options, especially for children and teens. Hospital emergency departments (ED’s) work to fill this gap in the short term, but ultimately ED’s are ill-equipped to respond to the magnitude of this crisis alone. A long-term strategy that treats and reimburses mental health at the same priority level as physical health is needed to ensure patients can receive timely access to care to the full continuum of behavioral health services.
We need a multifaceted approach to address the mental health crisis in our rural communities. But rather than solving these issues, some in Congress are pushing for harmful cuts that will damage already overburdened care resources. So-called “site-neutral” policies would cut funding to rural hospitals that are already struggling to recruit staff and provide much-needed care.
It’s unacceptable to cut funding from rural hospitals that play a critical role in mental health treatment and that work to ensure that it is readily available when rural Americans seek help. I urge Congress to work with rural communities to increase access to life-saving mental and other health care services. Rural America is counting on it.

